
Arthrosis of the joints is a chronic joint disease that develops due to metabolic disorders. As a result, degenerative, dystrophic changes and destruction of cartilage tissue occur.
It occurs inconspicuously, but often develops very quickly. A person begins to experience joint pain when moving, there is stiffness and decreased mobility, especially in the morning, while still "not at odds". If discomfort appears and periodic pain occurs during awkward movements or loads, it is very important to understand that this will not go away, and without intervention, the situation will only get worse.
osteoarthritis symptoms
Arthrosis of large and medium-sized joints seriously alters a person's lifestyle, worsens the quality and imposes restrictions. The development of the disease is like an avalanche and the treatment is most often associated with excruciating pain, and this is a clear sign of wear and tear on the joints.
The symptoms of osteoarthritis of the joints depend on how much the joint, cartilage tissue, and nearby tissues are affected.
In the early stages, arthrosis can be determined quite accurately, treatment in this case is sparing and does not require serious intervention and expensive drugs for the treatment of arthrosis.
types of arthrosis
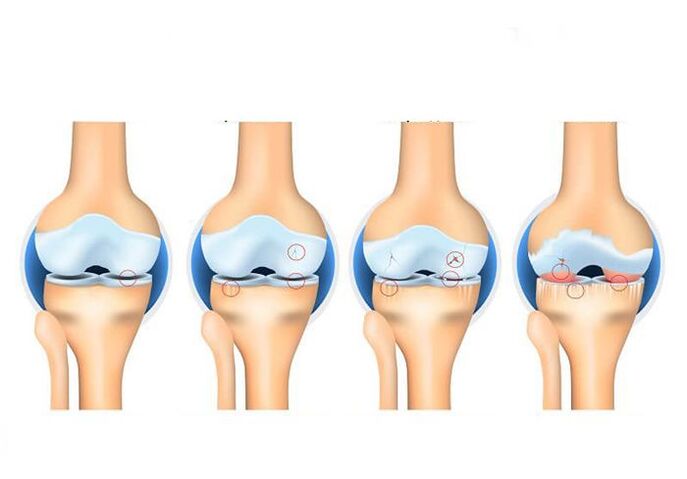
Arthrosis of the joints is classified according to several criteria. Depending on the degree of arthrotic changes in the cartilaginous tissue, 4 stages of arthrosis are distinguished. Osteoarthritis is also divided into primary and secondary. The cause of the development of primary arthrosis is age-related changes. Secondary osteoarthritis occurs due to joint injuries and diseases (eg, traumatic osteoarthritis or rheumatoid arthritis). The disease can also develop slowly over years or lead to joint destruction in just a few years (progressive osteoarthritis).
There are alsotypes of osteoarthritis, depending on the affected area:
- – osteoarthritis of the knee joint – osteoarthritis of the hip joint
- Uncovertebral arthrosis - arthrosis of the cervical vertebrae
- Vertebral osteoarthritis - damage to the spine
- Patellofemoral arthrosis is a type of gonarthrosis in which the patella and part of the femur suffer.
The degree of disease is determined by the degree of damage to cartilage tissue.
1st degree osteoarthritis - the cartilage tissue is slightly damaged, the person does not feel discomfort;
Grade II arthrosis - osteophytes appear, the space between the cartilages decreases, situational pain occurs with clumsy movements;
Grade III arthrosis - the cartilage tissue is destroyed in some places and exposes the bone tissue, the space between the cartilages decreases, the pain is frequent and intense;
Grade IV arthrosis - a significant part of the cartilaginous tissue is destroyed up to 60%, there is no space between the bones, patients experience constant and severe pain, hyperthermia of the area above the joint occurs.
- A characteristic seizure during movements and a slight background pain;
- Limited joint mobility, discomfort during full physical activity;
- Blood pressure indicators "jumping";
- Headache and dizziness;
- Convulsive syndrome and often muscle spasms;
- Visually observed deformity of the joint;
- Swelling, hyperthermia, or redness of the area of skin over the diseased joint;
- Violation of motor function.
Why does the disease appear?
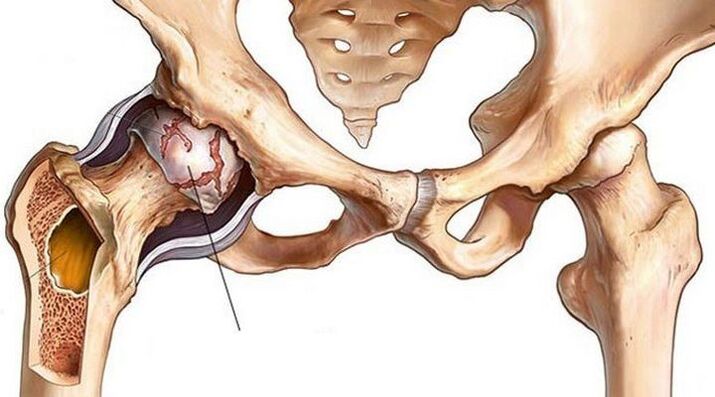
Arthrosis of the joints can manifest in any of the departments, but most often patients turn when osteoarthritis of the knee or hip joint makes itself felt. In the professional field, with a special and specific load on the hands, shoulder arthrosis can be observed.
Lesions differ in men and women.The strong half often suffers from temporomandibular joint, wrist, ankle and lumbar osteoarthritis. Women complain more about the thoracic and cervical regions, as well as the joints of the fingers and toes.
The type of disease is determined by the location of the lesion. There are the following types:
- arthrosis of the hip joint - coxarthrosis;
- arthrosis of the knee joint - gonarthrosis;
- damage to the patella and part of the femur - patellofemoral arthrosis (a type of gonarthrosis);
- spinal disease - vertebral arthrosis;
- damage to the cervical spine - discovered osteoarthritis.
The main reasons are:
- inflammatory process;
- professional sports;
- overweight;
- non-standard professional load, for example, squatting or kneeling;
- previous joint injuries (post-traumatic);
- hypothermia;
- heredity;
- age changes.
Osteoarthritis can appear as a standalone disease or it can be the result of a disease already in progress, so it's important to know a person's history.
Diagnosis of osteoarthritis of the joints
Arthrosis of the joints is detected by X-rays. The x-ray image shows how the joint is deformed and how much the joint space narrows. An MRI or arthroscopy may also be necessary, but only in particularly complex and ambiguous cases. Joint radiographs are usually sufficient to diagnose the disease.
To understand the presence of the disease, its severity, as well as what disorders led to the disease, a comprehensive diagnosis is carried out.
First, with the helpx-ray in different projectionsreceive information about the degree of damage to the joint.
Tomography (magnetic or computed resonance imaging) helpsexclude tumor processes.
Third, you needtake teststo understand whether arthrosis is an independent disease or a complication, as well as to determine the general condition of a person.
The study complex is the most informative and gives a clear idea of the degenerative-dystrophic changes and helps to choose the ideal treatment plan.
Osteoarthritis treatment
As discussed above, osteoarthritis can develop due to many factors, and the treatment plan is developed based on understanding the underlying causes and medications for treating osteoarthritis are selected accordingly.
Treatment should be developed individually, based on diagnostic results. Be sure to take into account the person's condition, their existing ailments.

Restoration of the articular surface and cartilage tissue is not rapid. Effective medications are prescribed with side effects. And taking medication to get the desired result lasts up to 6 months, so it's important to protect your health as much as possible from side effects.
Medical treatment of osteoarthritis
The main objective of this therapy is to remove the manifestations of arthrosis. Drug treatment of osteoarthritis of the joints includes:
- Non-steroidal anti-inflammatory drugs. With osteoarthritis, a person feels pain, the joint becomes inflamed. To eliminate unpleasant symptoms and stop inflammation, this group of drugs is prescribed.
- Hormonal injections into the joint. Corticosteroid drugs are most often administered in the acute phase of osteoarthritis.
- Chondroprotectors. The main task of these drugs is to stop the degenerative processes in the cartilage tissue to prevent its further destruction.
- Intra-articular injections of hyaluronic acid. Hyaluronic acid preparations are similar to synovial fluid in that they provide smooth gliding and free movement in the joint. With osteoarthritis, not enough synovial fluid is secreted, so orthopedists often prescribe hyaluronic acid injections (injections into the joint with osteoarthritis).
- Biological therapy of osteoarthritis (PRP and cytokine therapy). An innovative new method of osteoarthritis therapy, which has recently come into practice but is gaining in popularity. It is the use of drugs based on the patient's blood plasma enriched with platelets. Thanks to biological therapy, the blood supply to the joint is activated, the production of intra-articular fluid is activated, and the cartilage tissue is supplied with nutrients.
Important!Drug treatment of osteoarthritis is effective in the early stages of the disease. In addition, experts emphasize that drug therapy is not able to restore a damaged joint, but it will allow you to eliminate symptoms and slow the progression of osteoarthritis.
Physiotherapy and other conservative treatments for osteoarthritis
In the fight against osteoarthritis, physiotherapy is also used. Various procedures are prescribed (laser, phonophoresis, electrophoresis, magnetotherapy, UVT) and exercise therapy to improve metabolic processes and blood circulation, strengthen muscles.
Plus, with osteoarthritis, you just need to make a few lifestyle adjustments:
- Avoid overload - it is important to evenly distribute the activity and take breaks so as not to overload the joint
- Take care of your diet and monitor your weight - as excess weight only exacerbates the joint problem, you need to review your diet and reduce your body weight
- Remember to be careful and avoid injury as much as possible
- Use additional support for movement - in the later stages of osteoarthritis, independent movement becomes questionable, so you need to use a cane or crutches. For a more comfortable walk, you can also use orthopedic insoles - they will reduce the load on the joint.
There are also many folk recipes that "will help to defeat osteoarthritis". However, treating osteoarthritis at home also does not always bring results. In addition, the use of all kinds of lotions and ointments of their own preparation most often only provokes allergic reactions and does not affect the health of the joint.
Surgical treatment of osteoarthritis

How to treat osteoarthritis if all the above methods do not work? In this case, surgical treatment of osteoarthritis is prescribed. Depending on the degree of damage to the joint, the individual characteristics of each patient, a type of operation is selected.
Arthroscopy is a minimally traumatic intervention, an intra-articular operation through several micropunctures in the joint. With osteoarthritis, it is used as a temporary measure to "cleanse the joint": remove pieces of cartilage, osteophyte growths that interfere with free movement. Such treatment reduces joint pain, but is not a solution to the problem of osteoarthritis.
Osteotomy is an operation to align the axis of the joint. The fact is that with arthrosis, as a rule, a part of the joint suffers more (has a large load). As a result of the osteotomy, the load on the joint is redistributed. It should be noted that osteoarthritis is a progressive disease of the joints. Therefore, osteotomy is a way to delay treatment, but not to avoid it.
Joint arthroplasty is an effective and, in some cases, the only method of treating arthrosis of the joints. The essence of the operation is the removal of a joint destroyed by the disease and the implantation of an artificial endoprosthesis in its place. The artificial joint is individually selected, ideally adapted to each patient and fully restores the functions of the damaged joint after a period of rehabilitation.
Contraindications for osteoarthritis
What you need to pay attention to in arthrosis of the joints:
joint loads- with arthrosis, you need to give up lifting weights, excessive static loads. A cane can be used to unload the joint. Shoes – Well-fitting shoes reduce stress on the joint. It is advisable to avoid high heel shoes.
The weight- excess weight is another factor in the progression of osteoarthritis. Therefore, it is important to maintain a healthy weight and eat a balanced diet.
sportsalso needs to be reviewed. With arthrosis, it is necessary to exclude sudden movements (contact sports, wrestling), running long distances, lifting weights. But that doesn't mean that physical activity should be stopped completely. Moderate activity will only benefit the joint.
In addition to medical treatment, physiotherapy is actively used. These are magnetotherapy, electrotherapy, thermotherapy. In addition, physical therapy exercises are recommended to strengthen the muscles around the affected joint and improve blood supply.
A radical method to deform arthrosis, which has led to a deterioration in the quality of life, is often surgical intervention. In this case, arthroscopy or arthroplasty is performed.
Arthroscopy is a procedure in which the worn top layer of a joint is removed and a partial denture is placed in its place. This allows you to get rid of pain and restore mobility.
An endoprosthesis is the replacement of a joint with a prosthesis. It is suitable for severe destruction, when the joint itself does not make sense to save. The prosthesis has artificial cartilage, which anatomically corresponds fully to human ones.
Treatment of the disease in the early stage is the provision of high-quality nutrition to the cartilage tissue. Therefore, it is recommended to use chondroprotectors, preferably of natural origin, flavonoids. Motor load is also needed to improve blood supply to bones and perichondrium.
Knee deforming osteoarthritis
Deforming osteoarthritis of the knee joint(gonarthrosis, DAK) is a chronic progressive disease of the articular cartilage. It is characterized by the destruction of joint structures, accompanied by pain, inflammation and a characteristic curvature of the limb ("wheel legs" or X-shaped deformation).
Causes of deforming osteoarthritis of the knee
Without proper lubrication, the joint "dries up", cracks and loses height, exposing the heads of bones. In this case, the closing plate of the articular surface of the bone remains defenseless; re-irritation of the numerous nerve endings that are in it causes pain and discomfort.
The following factors or their combination can become the cause of deforming osteoarthritis of the knee:
- the presence of diseases of the joints (and knee - in particular) in relatives;
- genetic disorders associated with the formation of abnormal and unstable cartilage cells or their accelerated death;
- congenital and acquired malformations of the musculoskeletal system (flat feet, joint hypermobility, dysplasia, scoliosis, kyphosis and others);
- excessive professional, domestic or sports loads;
- microtraumas and injuries of the knee joint and meniscus, operations, leg fractures;
- circulatory disorders (varicose veins, atherosclerosis, thrombosis and other vascular diseases), their consequences (osteochondritis dissecans), as well as other causes of prolonged leg spasms;
- inflammatory diseases of the joints and periarticular tissues (synovitis, bursitis, tendinitis, arthritis), incl. autoimmune nature (rheumatoid arthritis, psoriatic);
- metabolic disorders (gout, diabetes mellitus);
- age-related processes of joint aging and calcium leaching from bones;
- hormonal disturbances and changes in the hormonal background (for example, associated with a lack of estrogen in women);
- hypovitaminosis;
- overweight (seen in ⅔ of patients);
- physical inactivity.
But the main reason why deforming osteoarthritis of the knee is so common is in its structure. The knee joint has only one axis (plane) of motion. Therefore, the scope of allowed moves is very limited. A clumsy turn can injure the periarticular tissues and trigger arthrotic changes - after all, the painful knee will be subject to daily stress.
The causes of the development of deforming arthrosis of the knee can be a large number of factors.

Symptoms of deforming arthrosis of the knee joint
Gradually increasing pain in the knee joint area. At first, the pain is noticeable only when moving - for example, with a straightening or sharp bending of the leg, there is a feeling that "unfortunately stepped on the foot". In the early stages, the pain may be episodic or so mild that it is perceived as discomfort. So the pain intensifies after physical exertion or a long stay in the same position. The skin also becomes painful - it reacts sensitively to any touch, incl. and clothes.
There are 3 types of specific pain in osteoarthritis deforming the knee joint:
- onset (lasts 15-30 minutes after the joint leaves a long resting state);
- mechanical (noticeable during physical activity and disappears after rest);
- block (feeling of a sharp twinge in the knee).
Symptoms of deforming arthrosis of the knee, as a rule, grow slowly due to the fact that the disease is not characterized by rapid progress. This is the insidious arthrosis - gradually getting used to the discomfort of the disease, the patient "gets used" to the pain, does not notice the deterioration and puts off the visit to the doctor.
Knowing the main symptoms of osteoarthritis of the knee will help to recognize the disease in time
Treatment of deforming arthrosis of the knee joint
The treatment of deforming arthrosis of the knee joint consists of the complex use of medications, dosed load on the joint, physiotherapeutic procedures and the use of orthopedic devices.
In the treatment process, it is extremely important to alternate loading and unloading to avoid static loading of the knee. Orthopedic insoles, specialized shoes, canes, crutches, walkers, ergonomic chairs for work and rest also help to delay the disease. Particularly effective are orthoses with variable stiffness, which make it possible to model the physiological axis of the leg and compensate for the deformity.
In the early stages of osteoarthritis deforming knee, the goal of treatment is to restore the destroyed joint and ligament apparatus, relieve pain, and increase the range of voluntary movements. In the later - in alleviating the patient's condition. For this, healing arthroscopy (washing with antiseptics) is performed when a piece of osteophyte is broken, corrective osteotomy (correction of a curved bone), endoprosthesis (replacement) of the joint.
In addition to the orthopedist, physical therapists and chiropractors, specialists in exercise therapy and massage therapy and surgeons will tell you how to treat deforming osteoarthritis of the knee joint.
The treatment of deforming arthrosis of the joints is a complex and time-consuming process that requires an integrated approach.

Physiotherapy
Among other physiotherapeutic methods for the treatment of deforming arthrosis of the knee joint, the following are used:
- laser and magnetotherapy;
- microwave therapy;
- shock wave therapy;
- amplipulse;
- ultrasound therapy;
- electrophoresis with analgine, novocaine, chymotrypsin, etc. ;
- phonophoresis with glucocorticoids;
- paraffin and ozokerite applications;
- cryotherapy;
- acupuncture;
- joint traction and kinesiotherapy;
- balneotherapy.
Massage for deforming osteoarthritis of the knee joint
Therapeutic massage and lymphatic drainage for deforming arthrosis of the knee joint, as well as manual therapy, are performed by a specialist after the inflammation in the joint has been relieved. For self-massage at home, caressing and rubbing is recommended, as well as movements aimed at stretching muscles and ligaments, a deep warm-up (performed last, after a warming effect). Self-massage combines well with local irritants and essential oils. Remember that with deforming osteoarthritis of the knee joint, massage is performed on both joints, even if only one of them is affected.
Exercises to deform arthrosis of the knee joints
Therapeutic gymnastics (exercise therapy) for deforming osteoarthritis of the knee joint is performed in a sitting or lying position, water aerobics is also effective. An individual set of exercises for deforming osteoarthritis of the knee joint is compiled by an instructor. Below, we offer a small warm-up aimed at strengthening the leg muscles.
- Sit on the floor, legs straight, emphasis on your hands behind your back. Bend and unfold your toes.
- The starting position is the same, slowly bend the leg, at the end of the movement supporting the toe on the floor. Repeat with the foot behind the other foot.
- Continuing in the same starting position, lift your extended leg in front of you, with your toes towards you.
- Without changing the starting position, we pull our hands to the toes of straight legs.
- Sitting on the floor, hug your bent knee and try to lift the other leg off the floor.
- Sitting on the floor, spread your legs shoulder-width apart. Turn your legs so that your toe moves 180 degrees.
- Sitting on the floor, legs bent. Roll the foot from heel to toe, feeling the work in the back of the thighs.
Great! Perform exercises to deform knee joint osteoarthritis at least 3-6 times a day.
Medications to deform knee arthrosis
Drug treatment of deforming osteoarthritis of the knee joint allows you to quickly stop the acute pain, reduce inflammation and swelling, and improve joint nutrition. Therefore, medications are used at all stages of the disease and help restore knee mobility.
chondroprotectors
Chondroprotectors in the form of tablets, capsules, sachets and injections are used to regenerate and maintain synovial cartilage.
Anti-inflammatory
Steroid and non-steroidal anti-inflammatory drugs are used to treat deforming osteoarthritis of the knee joint. They are prescribed in the form of pills, injections, sachets, creams, ointments and other products for external and internal use.
Anti-inflammatory medications can be used in conjunction with anesthetics, which are injected into the joint cavity as a block.
antispasmodics
Removal of the spasm is necessary to return the patient to normal activities and the normal supply of nutrients to the tissues.
Angioprotectors
To deform arthrosis of the knee joint, preparations based on horse chestnut and others are used.
heating agents
Among the heating agents, it is worth mentioning the preparations based on natural ingredients: snake and bee venom, pepper, mustard.
All these drugs improve the blood supply to the tissues and distract from pain.
Nutrition for deforming osteoarthritis of the knee
A healthy diet for osteoarthritis of the knee joint includes dishes low in trans fats and "fast" carbohydrates. Preference should be given to lean meats and fish, seafood and vegetables, steamed, in foil or cooked under a lid. Also useful are fruits, berries and antioxidant-rich drinks - wild plants, blueberries, blueberries, cranberries, high-quality green tea and coffee. You can also eat whole grains, vegetables.
But potatoes, white bread, sweets, convenience foods, fast food and alcohol should be excluded.
If you are overweight with osteoarthritis of the knee, consider low-carb diet options.

























